Healing Chronic Eczema
Patient Profile: Rohan M., 40-year-old male,
Condition: Severe eczema since age 5, with itchy, red patches on arms and legs, worsened by certain foods and stress. Topical steroids provided temporary relief but caused skin thinning.
Homeopathic Approach:
- A detailed history showed a link between eczema flares and dietary triggers like dairy, plus emotional stress from office
- Remedy: Sulphur 30C to address skin symptoms and underlying sensitivities, followed by Graphites for oozing patches.
- Dietary changes and stress-relief techniques, like journaling, were recommended.
Outcome: - After 2 months, itching reduced by 60%, and the skin began healing.
- By 5 months, Rohan’s skin was 80% clear, with no need for steroids.
- At the 1-year mark, flare-ups were minimal, occurring only with significant dietary lapses.

Healing Scabies
Scabies is a contagious skin condition caused by tiny mites that burrow into the skin, leading to intense itching and a rash. The mites, called Sarcoptes scabiei, tunnel under the skin to live, feed, and lay eggs, triggering an allergic reaction in the host. This reaction manifests as a rash, often with small, red bumps or spots, and severe itching, especially at night. Scabies is easily spread through prolonged skin-to-skin contact.
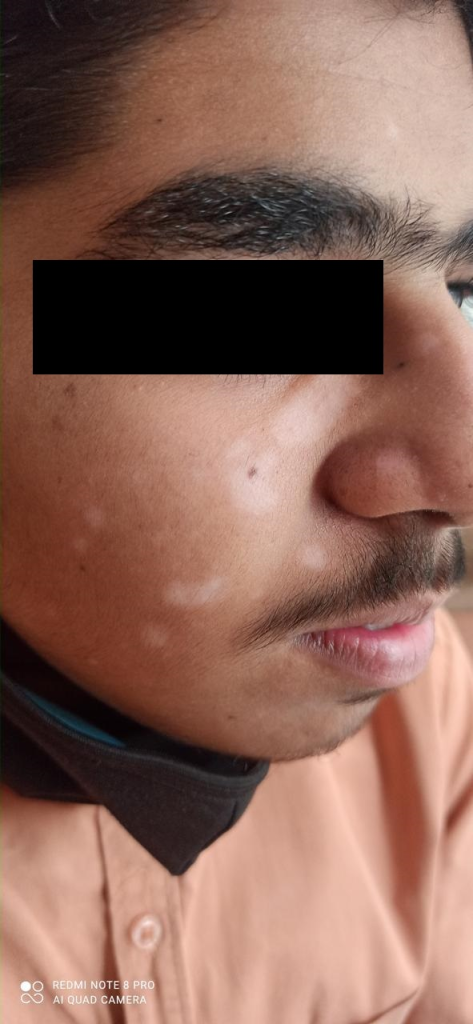
What is Leukoderma?
Leucoderma, also known as vitiligo, is a skin condition where patches of skin lose their pigment, resulting in white or depigmented areas. Below is a detailed overview based on available information:
What is Leukoderma?
- Definition: Leukoderma is a chronic skin disorder characterized by the loss of melanin, the pigment responsible for skin color, leading to white patches on the skin. It is often synonymous with vitiligo, though some sources distinguish leukoderma as depigmentation caused by external factors like injury or chemicals, while vitiligo is primarily autoimmune.
- Appearance: The condition manifests as pale, peachy, or white patches that can appear anywhere on the body. These patches are more noticeable in people with darker skin tones.
- Progression: Nonsegmental vitiligo (the most common form) tends to spread over time, affecting more areas, while segmental vitiligo is limited to one side or part of the body.
Causes
The exact cause of leucoderma/vitiligo is not fully understood, but several factors are implicated:
- Autoimmune Response: The immune system may attack melanocytes (pigment-producing cells), leading to melanin loss. This is a primary cause of vitiligo.
- Genetic Factors: Family history of vitiligo or other autoimmune disorders increases risk. Specific genes influence melanocyte stress and immune response.
- Environmental Triggers:
- Other Factors: Regional environmental risks, particularly early in life, or excessive mental worry may contribute.
Symptoms
- Primary Symptom: White or depigmented patches on the skin, often starting on hands, feet, or face.
- Associated Symptoms (more common in vitiligo):
- Psychosocial Impact: The visible patches can lead to social stigma or emotional distress, affecting self-esteem.

What is Ringworm?
- Definition: Ringworm (tinea) is a contagious fungal infection of the skin, hair, or nails caused by dermatophytes (e.g., Trichophyton, Microsporum). Despite the name, it’s not caused by a worm.
- Appearance: Circular, red, scaly patches with raised borders and a clearer center, resembling a ring. It may itch or burn.
- Common Sites: Scalp (tinea capitis), body (tinea corporis), feet (tinea pedis/athlete’s foot), groin (tinea cruris/jock itch), or nails (tinea unguium).
Causes
- Fungal Pathogens: Dermatophytes thrive in warm, moist environments.
- Transmission:
- Direct skin-to-skin contact with an infected person or animal (e.g., pets).
- Contact with contaminated surfaces (e.g., towels, floors, gym equipment).
- Poor hygiene or excessive sweating increases risk.
- Risk Factors: Living in humid climates, sharing personal items, or having a weakened immune system.
Symptoms
- Red, scaly, ring-shaped patches that may itch or burn.
- Scalp ringworm: Bald patches, scaling, or pustules.
- Nail ringworm: Thick, discolored, or brittle nails.
- Can spread to multiple areas if untreated.
Diagnosis
- Clinical Examination: A dermatologist identifies the characteristic ring-like rash.
- Tests:
- Skin scraping under a microscope (KOH test) to detect fungi.
- Fungal culture or Wood’s lamp exam for certain species.
- Differential Diagnosis: Must be distinguished from eczema, psoriasis, or leucoderma (vitiligo), which lacks scaling and itching.
Treatment
- Topical Antifungals (for mild cases):
- Creams or ointments like clotrimazole, miconazole, or terbinafine applied for 2–4 weeks.
- Available over-the-counter or by prescription.
- Oral Antifungals (for severe or scalp/nail infections):
- Medications like griseofulvin, terbinafine, or itraconazole, taken for weeks to months.
- Prescribed by a doctor due to potential side effects (e.g., liver issues).
- Home Care:
- Keep the area clean and dry.
- Avoid scratching to prevent spread or bacterial infection.
- Wash bedding, towels, and clothing regularly.
- Duration: Symptoms often improve within days of treatment, but completing the full course is essential to prevent recurrence.
Prevention
- Maintain good hygiene: Shower after sweating, dry skin thoroughly.
- Avoid sharing towels, combs, or clothing.
- Wear loose, breathable clothing and sandals in public showers or pools.
- Treat infected pets promptly.
- Disinfect surfaces in high-risk areas like gyms.
Complications
- Secondary bacterial infections from scratching.
- Permanent hair loss or scarring in severe scalp cases.
- Chronic nail damage if untreated.
Ringworm vs. Leucoderma
Since you previously asked about leucoderma, here’s a quick comparison to avoid confusion:
- Ringworm: Red, scaly, itchy, ring-shaped patches caused by fungi. Treatable with antifungals.
- Leucoderma/Vitiligo: White, non-itchy, depigmented patches due to melanin loss. Not contagious, managed with phototherapy or steroids, not curable.
- Ringworm is often mistaken for other rashes, but leucoderma’s lack of scaling or itching sets it apart.
When to See a Doctor
- If over-the-counter treatments fail after 2 weeks.
- If the rash spreads, involves the scalp/nails, or shows signs of infection (pus, swelling).
- For children or immunocompromised individuals, as oral medications may be needed.

What is Psoriasis?
Psoriasis is a chronic, autoimmune skin condition that causes rapid skin cell turnover, leading to thick, scaly patches on the skin. Below is a detailed overview, especially in light of your previous questions about leucoderma and ringworm, to clarify distinctions and provide comprehensive information.
- Definition: Psoriasis is a non-contagious, inflammatory condition where the immune system triggers excessive skin cell production, resulting in red, scaly, and sometimes itchy or painful patches (plaques).
- Appearance: Thick, red patches covered with silvery-white scales. Patches vary in size and may appear anywhere but commonly affect elbows, knees, scalp, lower back, and nails.
- Types:
- Plaque Psoriasis (most common): Raised, red patches with silvery scales.
- Guttate Psoriasis: Small, dot-like lesions, often triggered by infections like strep throat.
- Inverse Psoriasis: Smooth, red patches in skin folds (e.g., armpits, groin).
- Pustular Psoriasis: White, pus-filled blisters surrounded by red skin.
- Erythrodermic Psoriasis: Widespread redness and scaling, rare but severe.
- Psoriatic Arthritis: Psoriasis with joint inflammation, causing pain and stiffness.
Causes
- Autoimmune: The immune system mistakenly attacks healthy skin cells, accelerating their growth cycle (from 28–30 days to 3–4 days).
- Genetic Factors: Family history increases risk; specific genes (e.g., HLA-Cw6) are linked.
- Triggers:
- Stress, infections (e.g., strep throat), or skin injuries (cuts, burns, known as the Koebner phenomenon).
- Cold, dry weather or excessive sun exposure.
- Medications (e.g., beta-blockers, lithium) or alcohol/smoking.
- Hormonal changes or immune system disorders.
Symptoms
- Red, raised patches with silvery-white scales.
- Itching, burning, or soreness in affected areas.
- Dry, cracked skin that may bleed.
- Nail changes: Pitting, thickening, or separation from the nail bed.
- Joint pain or swelling (in psoriatic arthritis).
- Symptoms vary in severity, with flare-ups alternating with periods of remission.
Diagnosis
- Clinical Examination: A dermatologist assesses the appearance of skin, nails, and scalp. The presence of scaly plaques is often diagnostic.
- Medical History: To identify triggers, family history, or associated conditions.
- Skin Biopsy: Rarely needed but confirms psoriasis by showing thickened skin and immune cell infiltration.
- Differential Diagnosis: Must be distinguished from:
- Leucoderma/Vitiligo: White, non-scaly patches without inflammation.
- Ringworm: Red, ring-shaped, scaly patches caused by fungi, often itchier and treatable with antifungals.
- Eczema: Itchy, red, less scaly patches, often in skin folds.

Hair fall, or hair loss, is a common concern for both men and women, with varying causes, patterns, and treatments. Below is a detailed overview, tailored to address hair fall in males and females, considering your previous queries about skin conditions like leucoderma, ringworm, and psoriasis, which may be related to scalp or systemic issues.
Hair Fall
Overview of Hair Fall
- Definition: Hair fall refers to excessive shedding or loss of hair beyond the normal daily loss of 50–100 hairs. It can be temporary or permanent, depending on the cause.
- Patterns:
- Men: Often experience male pattern baldness (androgenetic alopecia), characterized by a receding hairline and thinning at the crown.
- Women: Typically experience diffuse thinning across the scalp (female pattern hair loss) or widening of the hair part, rarely leading to complete baldness.
Causes of Hair Fall
Causes vary by gender, but many are common to both men and women:
Common Causes in Both Genders
- Androgenetic Alopecia:
- Most common cause (70% of men, 40% of women by age 50).
- Men: Linked to dihydrotestosterone (DHT), a testosterone derivative, causing hair follicles to shrink.
- Women: Hormonal changes (e.g., menopause, PCOS) and genetics play a role; less DHT-driven.
- Telogen Effluvium:
- Temporary hair shedding due to stress, illness, childbirth, or nutritional deficiencies.
- Triggers: Emotional stress, surgery, rapid weight loss, or medications (e.g., antidepressants, beta-blockers).
- Nutritional Deficiencies:
- Lack of iron, zinc, biotin, vitamin D, or protein can weaken hair.
- Common in women with heavy menstrual cycles (iron deficiency) or restrictive diets.
- Scalp Conditions:
- Psoriasis: Scaly plaques on the scalp (from your previous query) can damage hair follicles if severe.
- Ringworm (tinea capitis): Fungal infection causing patchy hair loss, more common in children but possible in adults.
- Seborrheic Dermatitis: Dandruff-like condition causing scalp inflammation and hair fall.
- Leucoderma/Vitiligo: Rarely causes hair loss unless associated with autoimmune conditions like alopecia areata.
- Autoimmune Conditions:
- Alopecia Areata: Immune system attacks hair follicles, causing patchy hair loss in both genders.
- Linked to other autoimmune disorders (e.g., vitiligo, thyroid disease).
- Hormonal Imbalances:
- Men: High DHT levels or thyroid issues.
- Women: Polycystic ovary syndrome (PCOS), menopause, pregnancy, or thyroid disorders.
- Medications and Treatments:
- Chemotherapy, antidepressants, or blood thinners can cause hair shedding.
- Lifestyle Factors:
- Stress, smoking, poor sleep, or excessive hair styling (traction alopecia from tight hairstyles).
- Infections or Illness:
- Fungal infections (e.g., ringworm) or systemic illnesses like diabetes or lupus.
Gender-Specific Causes
- Men:
- Male Pattern Baldness: Genetic sensitivity to DHT, leading to receding hairline and crown thinning.
- Prostate Medications: Some drugs (e.g., finasteride) can paradoxically affect hair growth if misused.
- Women:
- Postpartum Hair Loss: Common after childbirth due to hormonal shifts.
- Menopause: Estrogen decline thins hair.
- PCOS: Excess androgens cause hair thinning on the scalp and excess hair on the face/body.
- Traction Alopecia: More common in women due to tight hairstyles (e.g., braids, ponytails).
Symptoms
- Men: Receding hairline, thinning crown, or partial/complete baldness in advanced stages.
- Women: Diffuse thinning, wider hair part, or reduced ponytail volume; rarely full baldness.
- General: Excessive hair on pillows, brushes, or shower drains; patchy bald spots (alopecia areata); scalp itching or scaling (if linked to psoriasis/ringworm).
Diagnosis
Trichoscopy: Magnified imaging of hair follicles.
Medical History: Assess family history, diet, stress, medications, or hormonal changes.
Physical Exam: Scalp inspection for inflammation, scaling (e.g., psoriasis, ringworm), or bald patterns.
Tests:
Pull Test: Gently pulling hair to assess shedding.
Blood Tests: Check for iron, ferritin, thyroid function, or vitamin deficiencies.
Scalp Biopsy: For suspected psoriasis, ringworm, or alopecia areata.
Female Health Care
Transforming Women’s Health with Advanced Homeopathy
With over 35 years of dedicated practice in Sri Ganganagar, Rajasthan, Dr. Parvinder Singh has brought relief and healing to countless women through advanced homeopathy. At Dr. Parvinder Homoeos, we believe in addressing the root causes of health issues with safe, natural, and individualized remedies. Below are inspiring success stories showcasing how our advanced homeopathic treatments have transformed lives by effectively managing common female health concerns.
Overcoming Menstrual Irregularities
Case: Anjali’s Story (Age 28, Sri Ganganagar)
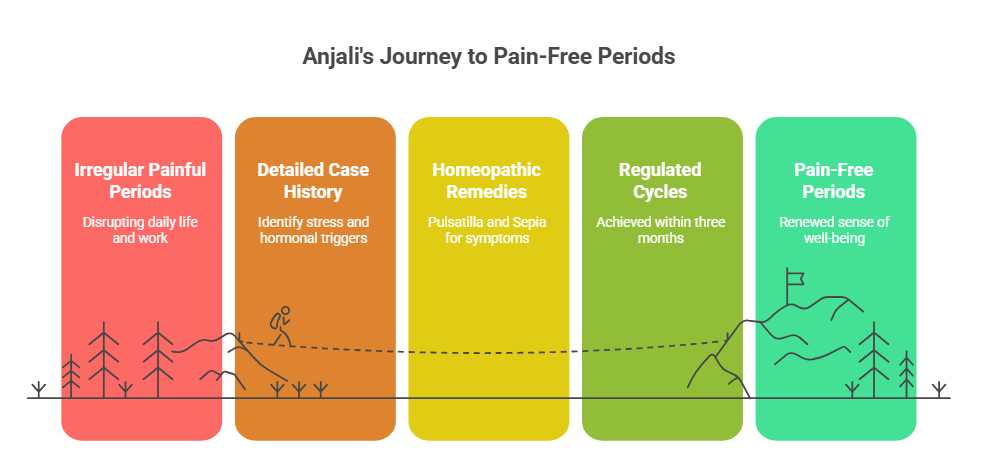
Anjali suffered from irregular and painful periods for years, impacting her daily life and work. Allopathic treatments provided temporary relief, but the pain and irregularity persisted. After consulting Dr. Parvinder Singh, a detailed case history revealed stress and hormonal imbalances as key triggers. Using advanced homeopathic remedies like Pulsatilla and Sepia, tailored to her unique symptoms, Dr. Parvinder helped regulate her cycles within three months. Today, Anjali enjoys pain-free periods and a renewed sense of well-being, crediting Dr. Parvinder’s holistic approach for her recovery.
Managing PCOS Naturally
Case: Priya’s Journey (Age 32, Hanumangarh)
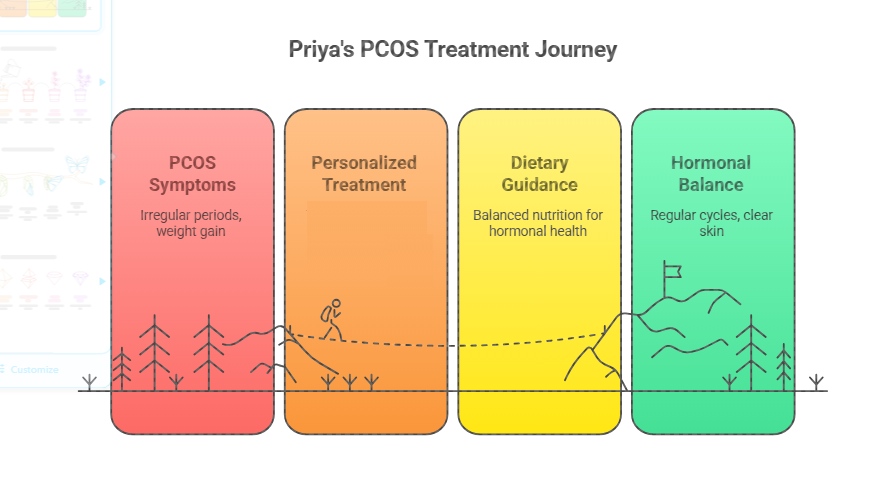
Priya was diagnosed with Polycystic Ovary Syndrome (PCOS), struggling with irregular periods, weight gain, and acne. Frustrated by conventional treatments, she turned to Dr. Parvinder Homoeos. Through a personalized treatment plan involving Thuja and Calcarea Carbonica, combined with dietary guidance, Priya’s symptoms improved significantly within six months. Her periods became regular, and her confidence soared as her skin cleared up. Priya’s story highlights how advanced homeopathy can address complex hormonal disorders without side effects.
Relief from Menopausal Symptoms
Case: Sunita’s Transformation (Age 50, Sri Ganganagar)
Sunita faced severe menopausal symptoms, including hot flashes, mood swings, and insomnia, which disrupted her quality of life. Seeking a natural alternative to hormone replacement therapy, she approached Dr. Parvinder. With remedies carefully selected after a thorough consultation, Sunita experienced a remarkable reduction in symptoms within two months. She now sleeps better, feels calmer, and recommends Dr. Parvinder’s care to every woman navigating menopause.
Resolving Uterine Fibroids
Case: Rekha’s Recovery (Age 40, Suratgarh)
Rekha was advised surgery for uterine fibroids causing heavy bleeding and pelvic pain. Hesitant about invasive procedures, she consulted Dr. Parvinder Singh. Using advanced homeopathic remedies like Fraxinus Americana and Calcarea Fluorica, Dr. Parvinder addressed her symptoms holistically. Within eight months, Rekha’s fibroids reduced in size, and her bleeding normalized, avoiding the need for surgery. Rekha praises Dr. Parvinder’s expertise and compassionate care for giving her a non-invasive solution.
Boosting Fertility Naturally
Case: Neha’s Dream Fulfilled (Age 35, Sri Ganganagar)
Neha and her husband struggled with infertility for five years, with no clear cause identified by conventional tests. Dr. Parvinder’s detailed evaluation pinpointed subtle hormonal and stress-related factors. With remedies, Neha’s health improved, and within a year, she conceived naturally. Now a proud mother, Neha credits Dr. Parvinder’s advanced homeopathy for making her dream of motherhood a reality.
Why Choose Dr. Parvinder Homoeos?
At Dr. Parvinder Homoeos, we combine 35+ years of experience with cutting-edge homeopathic techniques to provide safe, effective, and side-effect-free treatments. Our approach focuses on:
- Individualized Care: Each remedy is tailored to the patient’s unique physical, emotional, and mental symptoms.
- Holistic Healing: We address the root causes, not just symptoms, for lasting relief.
- Safe for All Ages: Our remedies are gentle, making them suitable for women at every stage of life, including pregnancy and menopause.
Take the First Step Toward Better Health
These success stories reflect the transformative power of advanced homeopathy under Dr. Parvinder Singh’s expertise. If you’re struggling with menstrual disorders, PCOS, menopausal symptoms, fibroids, infertility, or other women’s health issues, visit Dr parvinder homoeos.in to book a consultation. Let us help you reclaim your health naturally!
Description:
Medicine Selection: Choosing the appropriate homeopathic remedy based on symptoms.
Flowchart Steps:
Case-taking: Initial consultation to understand the patient’s symptoms and history.
General Information on Homeopathic Treatment for Asthma
Homeopathy offers a holistic and individualized approach to managing asthma, a chronic respiratory condition characterized by inflamed and narrowed airways, leading to symptoms like wheezing, breathlessness, chest tightness, and coughing. Unlike conventional treatments that often focus on symptom relief with inhalers or corticosteroids, homeopathy aims to address the root causes, including allergic tendencies and immune system imbalances, to provide long-term relief without side effects.
Key Aspects of Homeopathic Asthma Treatment:
- Individualized Remedies: Homeopathy tailors remedies to the patient’s unique symptoms, medical history, lifestyle, and triggers (e.g., allergens, stress, or exercise). No two asthma patients receive the same treatment, as remedies are selected based on individual characteristics.
- Common Remedies: Leading homeopathic medicines for asthma according to symptoms, age of problem current conditions etc.
- Holistic Approach: Homeopathy focuses on reducing airway inflammation, optimizing the immune system, and addressing triggers like stress or allergies. It aims to decrease the frequency and intensity of asthma episodes over time.
- Safety and Side Effects: Homeopathic remedies are derived from natural substances, highly diluted, and considered safe with no known side effects or dependency, unlike conventional medications like corticosteroids.
- Complementary Use: In acute asthma attacks, homeopathy can be used alongside conventional treatments (e.g., inhalers) for immediate relief, while long-term homeopathic treatment works to reduce dependency on such medications.
Treatment Process:
- Consultation: A detailed case history is taken, covering symptoms, triggers, family history, and lifestyle factors to identify the appropriate remedy.
- Personalized Plan: Remedies are prescribed based on the patient’s specific symptoms (e.g., wheezing worse at night or breathlessness triggered by cold air). Nutritional guidance and lifestyle changes may also be recommended.
- Duration: The treatment duration varies depending on the chronicity and severity of asthma, with some patients reporting significant improvement within months.